
Plantar Fasciitis
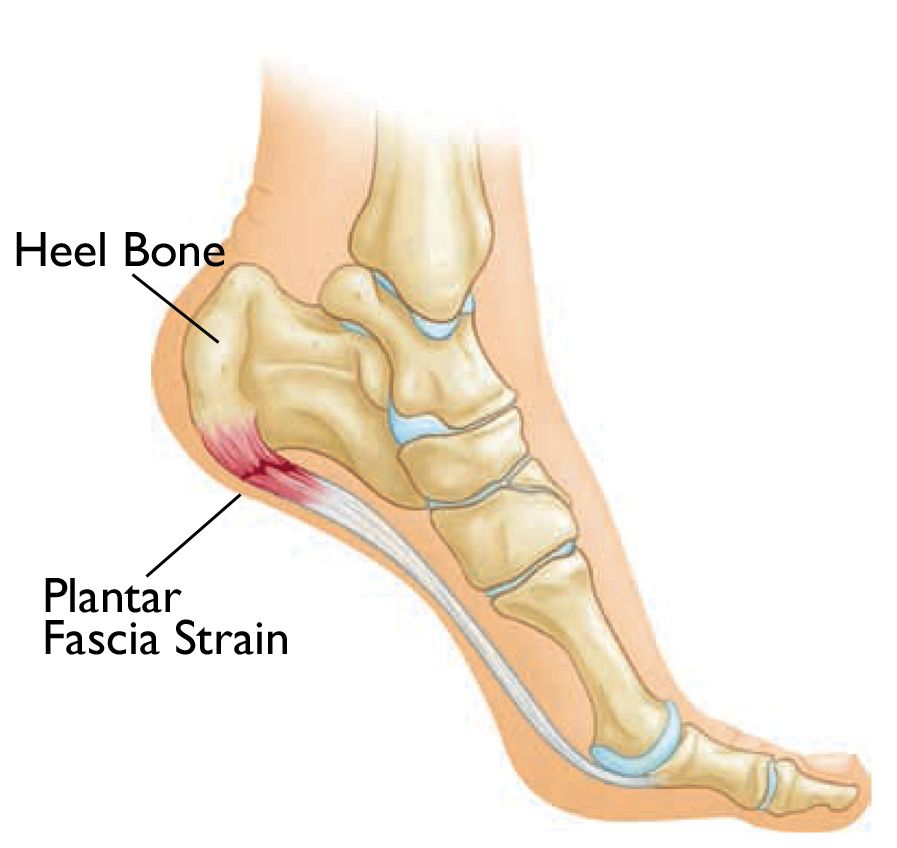
The plantar fascia is a thick band of tissue that runs from the front of the heel to the ball of the foot. It assists with the stabilization of the foot during the movement. However, when it strained and inflamed, it can cause the painful condition called plantar fasciitis. It is most often associated with sudden increased abnormal activity. Examples of such include running or similar, an overweight or sedentary lifestyle, repetitive strain, especially on hard surfaces, pronating feet or fallen arches and, possibly, ageing. Most often it is a pain under the heel that you experience when walking. Moreover, it gets worse when the patient is on their feet a long period of time. However, in some cases, it can ease a little after walking for a period.
Symptoms of Plantar Fasciitis
Symptoms develop gradually over time. It usually affects just one foot, but it can affect both feet.
Fascia is found throughout the body enveloping and linking muscles, bones and organs. In the foot it is a very tough connective tissue which runs from the heel to the bones in the middle of the foot and acts as a shock absorber, while supporting the arch of the foot in locomotion. This fascia continues to the calf muscles and hamstrings. Commonly the pain that is worse upon getting out of bed in the morning. Taking that first step may cause a sudden strain on the bottom of the foot. The pain can recur after long spells of sitting, but it tends to fade during exercise, once the area is warmed up.
Causes and Risk Factors
Even though plantar fasciitis can develop without an obvious cause, some factors can increase your risk of developing this condition. They include:
- Age. Plantar fasciitis is most common between the ages of 40 and 60.
- Certain types of exercise. Activities that place a lot of stress on your heel and attached tissue — such as long-distance running, ballet dancing and aerobic dance — can contribute to the onset of plantar fasciitis.
- Foot mechanics. Flat feet, tight achilles tendon, high-arched feet, or even an abnormal pattern of walking can affect the way weight is distributed when you’re standing and can put added stress on the plantar fascia.
- Obesity. Excess pounds put extra stress on your plantar fascia.
- Occupations that keep you on your feet. Factory workers, teachers and others who spend most of their work hours walking or standing on hard surfaces can damage the plantar fascia.
- Have injured their feet in some way, such as a stress fracture to one of the metatarsal bones.
How Can Osteopathy Help With Plantar Fasciitis?
There are many treatment options available for plantar fasciitis. But when it comes to treating this disorder you may want to consider the several benefits of Osteopathic care.
Treatment by Osteopath may:
Reduce stress in the ligament. To reduce inflammation you have to lower the stress placed on the ligament causing the tiny tears is the reason you are suffering from plantar fasciitis. If you do not take steps to reduce this stress, then pain and inflammation will continue to occur. Osteopathic manipulative treatment can help remove some of the stress from the ligament and give it an opportunity to heal through adjustments.
Minimise secondary injuries. Remember one of the things that can happen when you are suffering from this condition is a change in your gait to try to reduce the pain you experience. Using Osteopathic care as part of your treatment plan will help minimize the misalignments caused by a change in your gait. Misalignments that can cause problems in other parts of your body, like your feet, elbows, hips and lower back, if left untreated.
Osteopathic treatment focuses on understanding the development of plantar fasciitis rather than just treating this issue. Patients with mechanical problems of the hip, knee, pelvis, spine can end up with plantar fasciitis. Poor foot biomechanics often play a significant role in the cause of plantar fasciitis so it is vital to thoroughly assess and correct foot and leg biomechanics to prevent future plantar fasciitis episodes.
Your osteopath is trained in assessment of the musculoskeletal system which includes the feet. Osteopathic treatment offers a dynamic biomechanical hands on approach. Correction of mechanical problems of the hip, knee, pelvis, spine will contribute to an effective treatment for plantar fasciitis.

Several Tips To Help Treat Plantar Fasciitis At Home
Below are classic tips to help ease the pain and resolve the symptoms of plantar fasciitis at home.
- Ice It. While any icepack will do, freezing a plastic bottle full of water is a great at-home remedy. Place the frozen bottle on the floor and roll the foot backwards and forwards over it to ease the inflammation. This is especially good in the evening.
- Stretch And Strengthen. Stretching out your calf muscles, foot muscles, and buttock muscles can be useful in correction and prevention, along with stretching the Achilles Tendon and other leg muscles daily.
- Massage It. Using a tennis ball, or roll the ball under the sole of your foot, releasing the tension in the foot’s plantar fascia.
- Warm It Up. Before commencing strenuous exercise, stretching the foot can assist in releasing the plantar fascia.
- Choose Sensible Footwear. Wearing comfortable, supportive footwear is a must when suffering from plantar fasciitis; this means no bare feet and no high heels!
- Modify. Ask yourself a few questions to isolate why this condition has arisen now and see if you can modify your behaviour. For example; Why does only the right foot hurt? What have I done differently lately? Am I standing/walking for excessive periods? Am I wearing flip flops in the summertime?



